|
Overview
 We often think of fallen arches as a cause of foot pain, but they also stress your spine. In fact, fallen arches often contribute to unresolved or recurrent back pain. Excessive foot pronation (rolling in) can produce a short leg, pelvic unleveling, and increased curvature in your spine. Fallen arches place stress and strain on your feet, knees, hips, and spine. A custom orthotic can be a key part of your treatment plan in helping you get rid of your pain. Causes There are many reasons why flat feet develop. Here?s a look at some of the most common causes. Genetics, weak arches, injury, arthritis, diabetes, age, wear and tear on feet, tibialis posterior (ruptured tendon). Nervous system or muscle diseases such as cerebral palsy. Weakness and tightness of other muscles and tendons higher up in the lower extremity. The way our arches form depends on several factors. Our feet are complex structures that comprise twenty-six bones, thirty-three joints, and more than 100 muscles, tendons, and ligaments each. Each foot forms two arches. The arch that runs from the heel to the toe is known as the longitudinal arch, while the one that runs the width is known as the transverse arch. Ligaments (fibrous tissues) give our arches their shape and hold our bones together. The plantar fascia (the long, strong band of connective tissue that runs along the sole of your foot) and muscles add secondary support. There are also foot pads that absorb impact and assist with weight-bearing functions. How these things intertwine and work together determines the formation of our arches. A structural abnormality or injury to one of these components can result in flatfoot. Symptoms Pain along the inside of the foot and ankle, where the tendon lies. This may or may not be associated with swelling in the area. Pain that is worse with activity. High-intensity or high-impact activities, such as running, can be very difficult. Some patients can have trouble walking or standing for a long time. Pain on the outside of the ankle. When the foot collapses, the heel bone may shift to a new position outwards. This can put pressure on the outside ankle bone. The same type of pain is found in arthritis in the back of the foot. The symptoms of PTTD may include pain, swelling, a flattening of the arch, and an inward rolling of the ankle. As the condition progresses, the symptoms will change. For example, when PTTD initially develops, there is pain on the inside of the foot and ankle (along the course of the tendon). In addition, the area may be red, warm, and swollen. Later, as the arch begins to flatten, there may still be pain on the inside of the foot and ankle. But at this point, the foot and toes begin to turn outward and the ankle rolls inward. As PTTD becomes more advanced, the arch flattens even more and the pain often shifts to the outside of the foot, below the ankle. The tendon has deteriorated considerably and arthritis often develops in the foot. In more severe cases, arthritis may also develop in the ankle. Diagnosis Podiatrists are trained in expertly assessing flat feet and identifying different risk factors and the causes for it. Initial assessment will begin with a detailed history attempting to find out if any underlying illness has resulted in this. A detailed clinical examination normally follows. The patient may be asked to perform certain movements such as walking or standing on their toes to assess the function of the foot. Footwear will also be analysed to see if there has been excessive wear or if they are contributing to the pronation of the foot. To assess the structure of the foot further, the podiatrist may perform certain x-rays to get a detailed idea of the way the bones are arranged and how the muscle tissues may be affecting them. It also helps assess any potential birth defects in a bit more detail. pes planus exercises Non Surgical Treatment If you have fallen arches, but you are not experiencing any symptoms, then you probably do not need to seek treatment. If you are experiencing discomfort due to fallen arches, there are several treatment options. These treatment options include elevating the feet and applying ice to ease discomfort and reduce swelling, rest, exercises to stretch the feet, physical therapy, medication, such as anti-inflammatories, steroid injections and orthotic devices or customised arch supportsto wear in the shoes. If you have fallen arches and periodically experience pain related to that condition, it is a good idea to get orthotic devicesor custom arch supports, to wear in your shoes. The other treatment options, like medication and ice, will help to ease pain from fallen arches after you have already begun to experience pain. However, orthotic devices or(custom arch supports)can help to prevent pain from occurring at all. This preventative measure helps many people with fallen arches to avoid pain and prevent worsening of their condition. In severe cases of fallen arches, surgery may be required to correct the problem. You can also help to prevent pain and exacerbation of fallen arches by reducing your risk factors. If you are overweight, try to lose weight. Even a small weight loss can reduce the pressure on your feet significantly. If you are diabetic, manage your blood sugar as best as possible. Losing weight often also improves the condition of diabetics. You should also avoid high-impact activities, like running on the road, tennis, and sports that involve jumping. Try a gentler form of exercise, like swimming, instead. If you have fallen arches, orthotic devices or(custom arch supports)are an important component of your treatment and can help to prevent pain. Surgical Treatment  Since there are many different causes of flatfoot, the types of flatfoot reconstruction surgery are best categorized by the conditions. Posterior tibial tendon dysfunction. In this condition, the tendon connecting the calf muscle to the inner foot is torn or inflamed. Once the tendon is damaged it no longer can serve its main function of supporting the arch of the foot. Flatfoot is the main result of this type of condition and can be treated by the following flatfoot reconstruction surgeries. Lengthening of the Achilles tendon. Otherwise known as gastrocnemius recession, this procedure is used to lengthen the calf muscles in the leg. This surgery treats flatfoot and prevents it from returning in the future. This procedure is often combined with other surgeries to correct posterior tibial tendon dysfunction. Cleaning the tendon. Also known as tenosynovectomy, this procedure is used in the earlier and less severe stages of posterior tibial tendon dysfunction. It is performed before the arch collapses and while the tendon is only mildly affected. The inflamed tissue is cleaned away and removed from the remaining healthy tendon. Tendon transfer. This procedure is done to correct flatfoot and reform the lost arch in the foot. During the procedure, the diseased tendon is removed and replaced by tendon from another area of the foot. If the tendon is only partially damaged, the inflamed part is cleaned and removed then attached to a new tendon. Cutting and shifting bones. Also called an osteotomy, this procedure consists of cutting and reconstructing bones in the foot to reconstruct the arch. The heel bone and the midfoot are most likely reshaped to achieve this desired result. A bone graft may be used to fuse the bones or to lengthen the outside of the foot. Temporary instrumentation such as screws and plates can also be used to hold the bones together while they heal. Prevention Well-fitted shoes with good arch support may help prevent flat feet. Maintaining a healthy weight may also lower wear and tear on the arches. Overview
Many people undergo surgery for various reasons - arthritis, knee replacement, hip replacement, even back surgery. However, the underlying cause of leg length inequality still remains. So after expensive and painful surgery, follow by time-consuming and painful rehab, the true culprit still remains. Resuming normal activities only continues to place undue stress on the already overloaded side. Sadly so, years down the road more surgeries are recommended for other joints that now endure the excessive forces.  Causes The causes of LLD are many, including a previous injury, bone infection, bone diseases (dysplasias), inflammation (arthritis) and neurologic conditions. Previously broken bones may cause LLD by healing in a shortened position, especially if the bone was broken in many pieces (comminuted) or if skin and muscle tissue around the bone were severely injured and exposed (open fracture). Broken bones in children sometimes grow faster for several years after healing, causing the injured bone to become longer. Also, a break in a child?s bone through a growth center (located near the ends of the bone) may cause slower growth, resulting in a shorter extremity. Bone infections that occur in children while they are growing may cause a significant LLD, especially during infancy. Bone diseases may cause LLD, as well; examples are neurofibromatosis, multiple hereditary exostoses and Ollier disease. Inflammation of joints during growth may cause unequal extremity length. One example is juvenile rheumatoid arthritis. Osteoarthritis, the joint degeneration that occurs in adults, very rarely causes a significant LLD. Symptoms Often there are few or no symptoms prior to the age of 25-35. The most common symptom is chronic lower back pain, but also is frequently middle and upper back pain. Same-sided and repeated injury or pain to the hip, knee and/or ankle is also a hallmark of a long-standing untreated LLD. It is not uncommon to have buttock or radiating hip pain that is non-dermatomal (not from a disc) and tends to go away when lying down. Diagnosis There are several orthopedic tests that are used, but they are rudimentary and have some degree of error. Even using a tape measure with specific anatomic landmarks has its errors. Most leg length differences can be seen with a well trained eye, but I always recommend what is called a scanagram, or a x-ray bone length study (see picture above). This test will give a precise measurement in millimeters of the length difference. Non Surgical Treatment Treatment depends on what limb has the deformity and the amount of deformity present. For example, there may be loss of function of the leg or arm. Cosmetic issues may also be a concern for the patient and their family. If there are problems with the arms, the goal is to improve the appearance and function of the arm. Treatment of leg problems try to correct the deformity that may cause arthritis as the child gets older. If the problem is leg length, where the legs are not "equal," the goal is equalization (making the legs the same length). Treatment may include the use of adaptive devices, prosthesis, orthotics or shoe lifts. If the problem is more severe and not treatable with these methods, then surgery may be necessary.  height increase medicine Surgical Treatment Limb deformity or leg length problems can be treated by applying an external frame to the leg. The frame consists of metal rings which go round the limb. The rings are held onto the body by wires and metal pins which pass through the skin and are anchored into the bone. During this operation, the bone is divided. Gradual adjustment of the frame results in creation of a new bone allowing a limb to be lengthened. The procedure involves the child having an anaesthetic. The child is normally in hospital for one week. The child and family are encouraged to clean pin sites around the limb. The adjustments of the frame (distractions) are performed by the child and/or family. The child is normally encouraged to walk on the operated limb and to actively exercise the joints above and below the frame. The child is normally reviewed on a weekly basis in clinic to monitor the correction of the deformity. The frame normally remains in place for 3 months up to one year depending on the condition which is being treated. The frame is normally removed under a general anaesthetic at the end of treatment. Overview
 Heel pain is usually felt either under the heel or just behind it. Heel pain has a prevalence of 3.6%. US studies estimate that 7% of older adults report tenderness under the heel. Plantar fasciitis is estimated to account for 8% of all running-related injuries. There are 26 bones in the human foot, of which the heel is the largest. Pain typically comes on gradually, with no injury to the affected area. It is often triggered by wearing a flat shoe. In most cases the pain is under the foot, towards the front of the heel. The majority of patients recover with conservative treatments within months. Home care such as rest, ice, proper-fitting footwear and foot supports are often enough to ease heel pain. To prevent heel pain, it's recommended to reduce the stress on that part of the body. Causes Common causes of heel pain include, Heel Spurs, a bony growth on the underside of the heel bone. The spur, visible by X-ray, appears as a protrusion that can extend forward as much as half an inch. When there is no indication of bone enlargement, the condition is sometimes referred to as "heel spur syndrome." Heel spurs result from strain on the muscles and ligaments of the foot, by stretching of the long band of tissue that connects the heel and the ball of the foot, and by repeated tearing away of the lining or membrane that covers the heel bone. These conditions may result from biomechanical imbalance, running or jogging, improperly fitted or excessively worn shoes, or obesity. Plantar Fasciitis, both heel pain and heel spurs are frequently associated with plantar fasciitis, an inflammation of the band of fibrous connective tissue (fascia) running along the bottom (plantar surface) of the foot, from the heel to the ball of the foot. It is common among athletes who run and jump a lot, and it can be quite painful. The condition occurs when the plantar fascia is strained over time beyond its normal extension, causing the soft tissue fibers of the fascia to tear or stretch at points along its length; this leads to inflammation, pain, and possibly the growth of a bone spur where the plantar fascia attaches to the heel bone. The inflammation may be aggravated by shoes that lack appropriate support, especially in the arch area, and by the chronic irritation that sometimes accompanies an athletic lifestyle. Resting provides only temporary relief. When you resume walking, particularly after a night's sleep, you may experience a sudden elongation of the fascia band, which stretches and pulls on the heel. As you walk, the heel pain may lessen or even disappear, but that may be just a false sense of relief. The pain often returns after prolonged rest or extensive walking. Heel pain sometimes results from excessive pronation. Pronation is the normal flexible motion and flattening of the arch of the foot that allows it to adapt to ground surfaces and absorb shock in the normal walking pattern. As you walk, the heel contacts the ground first; the weight shifts first to the outside of the foot, then moves toward the big toe. The arch rises, the foot generally rolls upward and outward, becoming rigid and stable in order to lift the body and move it forward. Excessive pronation-excessive inward motion-can create an abnormal amount of stretching and pulling on the ligaments and tendons attaching to the bottom back of the heel bone. Excessive pronation may also contribute to injury to the hip, knee, and lower back. Pain at the back of the heel is associated with Achilles tendinitis, which is inflammation of the Achilles tendon as it runs behind the ankle and inserts on the back surface of the heel bone. It is common among people who run and walk a lot and have tight tendons. The condition occurs when the tendon is strained over time, causing the fibers to tear or stretch along its length, or at its insertion on to the heel bone. This leads to inflammation, pain, and the possible growth of a bone spur on the back of the heel bone. The inflammation is aggravated by the chronic irritation that sometimes accompanies an active lifestyle and certain activities that strain an already tight tendon. Other possible causes of heel pain include rheumatoid arthritis and other forms of arthritis, including gout, which usually manifests itself in the big toe joint, an inflamed bursa (bursitis), a small, irritated sac of fluid; a neuroma (a nerve growth); or other soft-tissue growth. Such heel pain may be associated with a heel spur or may mimic the pain of a heel spur. Haglund's deformity ("pump bump"), a bone enlargement at the back of the heel bone in the area where the Achilles tendon attaches to the bone. This sometimes painful deformity generally is the result of bursitis caused by pressure against the shoe and can be aggravated by the height or stitching of a heel counter of a particular shoe, a bone bruise or contusion, which is an inflammation of the tissues that cover the heel bone. A bone bruise is a sharply painful injury caused by the direct impact of a hard object or surface on the foot. Symptoms The heel can be painful in many different ways, depending on the cause. Plantar fasciitis commonly causes intense heel pain along the bottom of the foot during the first few steps after getting out of bed in the morning. This heel pain often goes away once you start to walk around, but it may return in the late afternoon or evening. Although X-ray evidence suggests that about 10% of the general population has heels spurs, many of these people do not have any symptoms. In others, heel spurs cause pain and tenderness on the undersurface of the heel that worsen over several months. In a child, this condition causes pain and tenderness at the lower back portion of the heel. The affected heel is often sore to the touch but not obviously swollen. Bursitis involving the heel causes pain in the middle of the undersurface of the heel that worsens with prolonged standing and pain at the back of the heel that worsens if you bend your foot up or down. Pump bump, this condition causes a painful enlargement at the back of the heel, especially when wearing shoes that press against the back of the heel. Heel bruises, like bruises elsewhere in the body, may cause pain, mild swelling, soreness and a black-and-blue discoloration of the skin. Achilles tendonitis, this condition causes pain at the back of the heel where the Achilles tendon attaches to the heel. The pain typically becomes worse if you exercise or play sports, and it often is followed by soreness, stiffness and mild swelling. A trapped nerve can cause pain, numbness or tingling almost anywhere at the back, inside or undersurface of the heel. In addition, there are often other symptoms, such as swelling or discoloration - if the trapped nerve was caused by a sprain, fracture or other injury. Diagnosis The diagnosis of heel pain and heel spurs is made by a through history of the course of the condition and by physical exam. Weight bearing x-rays are useful in determining if a heel spur is present and to rule out rare causes of heel pain such as a stress fracture of the heel bone, the presence of bone tumors or evidence of soft tissue damage caused by certain connective tissue disorders. Non Surgical Treatment Treatments to add to your stretching program include wearing good-quality shoes, icing the painful area, and massaging the arch. Do not walk barefoot; walk in shoes with good heel and arch supports such as high-quality walking or running shoes. Keep a pair of shoes next to your bed so you can put them on before taking your first step. Your doctor may recommend that you wear an additional arch support or a heel cup in the shoes. Icing your foot can help relieve pain. Rub a frozen bottle of water or an ice cup over the tender areas for five minutes two times each day. Massage your foot by rolling a tennis, golf ball, or baseball along your sole and heel. This friction massage can help break up adhesions and stretch the plantar fascia. Do this for five minutes two times each day. If you are a runner or just started a walking or running program, evaluate your training for errors such as warming up improperly, increasing mileage too quickly, running hills excessively, running on surfaces that are too hard, or wearing broken down shoes. Adjusting your training program can help relieve your pain. While recovering from heel pain, walk or jog in a pool or crosstrain by biking and swimming. These activities maintain your cardiovascular fitness without stressing your heel cord or plantar fascia. Heel pain takes time to go away. Be patient and remember that no treatment is a substitute for STRETCHING! Surgical Treatment Surgery is a last resort in the treatment of heel pain. Physicians have developed many procedures in the last 100 years to try to cure heel pain. Most procedures that are commonly used today focus on several areas, remove the bone spur (if one is present), release the plantar fascia (plantar fasciotomy), release pressure on the small nerves in the area. Usually the procedure is done through a small incision on the inside edge of the foot, although some surgeons now perform this type of surgery using an endoscope. An endoscope is a tiny TV camera that can be inserted into a joint or under the skin to allow the surgeon to see the structures involved in the surgery. By using the endoscope, a surgeon can complete the surgery with a smaller incision and presumably less damage to normal tissues. It is unclear whether an endoscopic procedure for this condition is better than the traditional small incision. Surgery usually involves identifying the area where the plantar fascia attaches to the heel and releasing the fascia partially from the bone. If a small spur is present this is removed. The small nerves that travel under the plantar fascia are identified and released from anything that seems to be causing pressure on the nerves. This surgery can usually be done on an outpatient basis. This means you can leave the hospital the same day. heel spur surgery Prevention 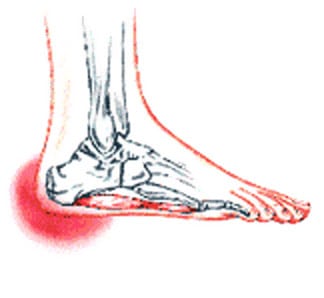 Wearing real good, supportive shoes are a great way to avoid heel pain. Usually, New Balance is a good shoe to wear, just for everyday shoe gear. By wearing proper footwear and performing thorough stretches, athletes can help prevent frequent heel pain. If you are starting to get a little discomfort or pain in the feet or heel, know that pain is not normal. So if you are having pain, you should be proactive and visit our office. If you let heel pain get out of control you could run into several other problems. It is always suggested to visit a podiatrist whenever you are experiencing pain. Overview
Causes In many cases, a neuroma may develop as a result of excessive loading on the front of the foot. Sometimes, a patient?s anatomic alignment in the forefoot contributes to the overload. There may be some cases where the neuroma develops spontaneously, for no obvious reason. However, once the nerve is irritated, pressure from walking, and from the adjacent bony prominences (metatarsal heads), as well as from the intermetatarsal ligament that binds the heads together, all may contribute to persistent pain. Repetitive pressure on the nerve causes localized injury with resulting scarring and fibrosis of the nerve. This leads to symptoms in the distribution of the nerve. Symptoms If you have a Morton?s neuroma, you may have one or more of these symptoms where the nerve damage is occurring, Tingling, burning, or numbness, pain, a feeling that something is inside the ball of the foot or a feeling that there?s something in the shoe or a sock is bunched up. The progression of a Morton?s neuroma often follows the following pattern. The symptoms begin gradually. At first they occur only occasionally, when wearing narrow-toed shoes or performing certain aggravating activities. The symptoms may go away temporarily by removing the shoe, massaging the foot, or by avoiding aggravating shoes or activities. Over time the symptoms progressively worsen and may persist for several days or weeks. The symptoms become more intense as the neuroma enlarges and the temporary changes in the nerve become permanent. Diagnosis The diagnosis of interdigital neuroma is usually made by physical examination and review of the patient's medical history.MRI ad High Definition Ultrasound examination may be useful to confirm the diagnoses however they may still not be 100% reliable. The commonest reason for this is de to natural substances present in between the metatarsal heads and between the fat pad and the intermetatarsal ligament. These natural substances i.e. bursa, fat, capsular thickening and even bony growths, can all be a factor in the impingement process and may need to be surgically cleared. Non Surgical Treatment The first line of treatment is to try modifying footwear. Often simply wearing broader fitting shoes can reduce pressure on the neuroma and so reduce pain. Orthotic inserts can also help as they can again help reduce pressure on certain parts of the foot. Padding and taping the toe area is another option. In some cases a steroid injection into the foot may be suggested. This can be done as a day case without the need for anaesthesia and helps reduce inflation of the nerve. It can halt the pain in round 70 % of cases. Sometimes a combination of alcohol and local anaesthesia may be injected as this helps reduce pain.  Surgical Treatment Should the problem have progressed beyond the point where these measures are sufficient, the podiatric professional may recommend surgery. This procedure involves excision of the involved nerve mass. This will relieve the pain. Many patients report permanent numbness in the spot formerly affected by the neuroma, but prefer it to the pain. Most surgeries are successful; unfortunately, there are cases where the patient suffers another neuroma, sometimes in or near the same spot as before. A podiatric professional can explain the statistics of recurrence in various cases. If you suspect a neuroma, don?t wait for it to get better on its own. The earlier the diagnosis, the higher the likelihood that it can be treated with conservative measures. Don?t think that foot pain of any kind is inevitable, either, even if it runs in your family. Overview
The accessory navicular also termed the os navicularum or os tibiale externum - is an extra bone or piece of cartilage on the inner side of the foot above the arch that attaches to the posterior tibial tendon within this area. This extra bone, present at birth, is not part of the normal bone structure and found in approximately 10% of the population. Some people with an accessory navicular may be unaware of the condition if symptoms are never experienced. But accessory navicular syndrome is a painful condition caused by aggravating the bone, the posterior tibial tendon or both.Accessory navicular syndrome is an irritation of the accessory navicular and/or posterior tibial tendon. This irritation can be caused by shoe rubbing, trauma, excessive activity, or overuse and can cause problems with the shape and function of your foot. Many people with this disorder also have flat feet which puts more strain on the posterior tibial tendon. Some people are born with an accessory Navicular because during development, the bones of the feet sometimes develop abnormally causing the extra bone to form on the inside of the foot.  Causes People who have an accessory navicular often are unaware of the condition if it causes no problems. However, some people with this extra bone develop a painful condition known as accessory navicular syndrome when the bone and/or posterior tibial tendon are aggravated. This can result from any of the following. Trauma, as in a foot or ankle sprain. Chronic irritation from shoes or other footwear rubbing against the extra bone. Excessive activity or overuse. Symptoms Adolescence is a common time for the symptoms to first appear. This is a time when bones are maturing and cartilage is developing into bone. Sometimes, however, the symptoms do not occur until adulthood. The signs and symptoms of accessory navicular syndrome include a visible bony prominence on the midfoot (the inner side of the foot, just above the arch) Redness and swelling of the bony prominence. Vague pain or throbbing in the midfoot and arch, usually occurring during or after periods of activity. Diagnosis To diagnose accessory navicular syndrome, the foot and ankle surgeon will ask about symptoms and examine the foot, looking for skin irritation or swelling. The doctor may press on the bony prominence to assess the area for discomfort. Foot structure, muscle strength, joint motion, and the way the patient walks may also be evaluated. X-rays are usually ordered to confirm the diagnosis. If there is ongoing pain or inflammation, an MRI or other advanced imaging tests may be used to further evaluate the condition. Non Surgical Treatment Excess weight will increase the force on the posterior tibial tendon as it inserts into the accessory navicular and will tend to precipitate or aggravate symptoms. If a patient with a symptomatic accessory navicular is overweight, then losing weight can be very helpful. Even losing 5-10lbs will decrease the amount of force going through the foot with each step by as much as 15-30lbs. This is because the foot acts like a lever serving to magnify the force absorbed by the foot with each step.  Surgical Treatment Surgery may be an option if non-surgical treatment does not decrease the symptoms of accessory navicular syndrome. Since this bone is not needed for the foot to function normally, Your surgeon may remove the accessory navicular, reshape the area, and repair the posterior tibial tendon for improved function. Overview
Some people have more bones in their feet than others. Actually, it?s not all that uncommon to have extra bones in the feet. These extra bones area called accessory bones. The navicular bone, one of the small bones located at the instep or arch of the middle of the foot, is an example of an extra bone people are born with. It?s called the accessory navicular bone. During the maturation process, the navicular and the accessory navicular never fuse into one solid bone, but remain connected by fibrous tissue or cartilage. It is estimated that 4-14% of the population are born with an accessory navicular bone.  Causes Most of the time, this condition is asymptomatic and people may live their whole lives unaware that they even have this extra bone. The main reason the accessory navicular bone becomes problematic is when pain occurs. There is no need for intervention if there is no pain. The accessory navicular bone is easily felt in the medial arch because it forms a bony prominence there. Pain may occur if the accessory bone is overly large causing this bump on the instep to rub against footwear. Symptoms Adolescence is a common time for the symptoms to first appear. This is a time when bones are maturing and cartilage is developing into bone. Sometimes, however, the symptoms do not occur until adulthood. The signs and symptoms of accessory navicular syndrome include A visible bony prominence on the midfoot (the inner side of the foot, just above the arch) Redness and swelling of the bony prominence. Vague pain or throbbing in the midfoot and arch, usually occurring during or after periods of activity. Diagnosis Accessory navicular syndrome is diagnosed by asking about symptoms and examining the foot for skin irritation and swelling. Doctors may assess the area for discomfort by pressing on the bony prominence. Foot structure, muscle strength, joint motion and walking patterns may also be evaluated. Non Surgical Treatment Most doctors will try to find a non-surgical approach to the issue due to costs and complications involved in a surgery. Some non-surgical procedures are: Immobilization which consists of placing the foot in a cast or walking boot to allow rest and decrease inflammation, placing a towel-covered-icepack on the area to reduce inflammation, anti-inflammatory or steroid drugs/injections may be prescribed to reduce swelling and pain, physical therapy may be used to help strengthen muscles and prevent a reoccurrence of symptoms, Orthotic Devices placed in the shoe to help support the arch and prevent a reoccurrence of symptoms.  Surgical Treatment Fusion of the accessory navicular to the navicular with screws is required when there is a large accessory navicular bone and removal of this bone would reduce the articular surface of the Navicular to the talus (coxa pedis). Fusion will relieve pain without disrupting the tibialis posterior tendon insertion nor narrowing talar head support. In most instances, a patient’s recovery will be as follows. 0-6 weeks: Immobilization (in case or cast boot) non-weight-bearing or touch weight-bearing. 6-10 weeks: Increasing activity in a cast boot. Physical therapy to work on strength and balance. Full recovery after 9 weeks-2 months. In some patients (where the posterior tibial tendon is still intact and functioning) the treating surgeon may allow weight-bearing as tolerated in a cast boot immediately after surgery. Overview
An accessory navicular is defined as an extra bone in the foot, and oftentimes it causes moderate to severe discomfort. Depending on the severity, your doctor may recommend a non-surgical treatment to alleviate the pain, or surgery if treatment doesn?t decrease symptoms.  Causes People who have an accessory navicular often are unaware of the condition if it causes no problems. However, some people with this extra bone develop a painful condition known as accessory navicular syndrome when the bone and/or posterior tibial tendon are aggravated. This can result from any of the following. Trauma, as in a foot or ankle sprain. Chronic irritation from shoes or other footwear rubbing against the extra bone. Excessive activity or overuse. Symptoms What precipitates the pain? It will usually be caused by rubbing of the skate or other footwear against the prominence. You?ll commonly see blisters or a red irritated area. Other symptoms to look for, especially when you?re treating an older child or adult, include an area of pain along the posterior tibial tendon of the arch and fatigue of the legs. Typically, these patients are not able to participate in sports for a lengthy period of time or you?ll hear them complain of pain and/or soreness after extended activities. Most individuals with a prominent navicular area will have tried accommodating this area with a doughnut pad or adjustments to their skate. Diagnosis To diagnose accessory navicular syndrome, medical staff ask about the patient?s activities and symptoms. They will examine the foot for irritation or swelling. Medical staff evaluate the bone structure, muscle, joint motion, and the patient?s gait. X-rays can usually confirm the diagnosis. MRI or other imaging tests may be used to determine any irritation or damage to soft-tissue structures such as tendons or ligaments. Because navicular accessory bone irritation can lead to bunions, heel spurs and plantar fasciitis, it?s important to seek treatment. Non Surgical Treatment The goal of non-surgical treatment for accessory navicular syndrome is to relieve the symptoms. The following may be used. Immobilization. Placing the foot in a cast or removable walking boot allows the affected area to rest and decreases the inflammation. Ice. To reduce swelling, a bag of ice covered with a thin towel is applied to the affected area. Do not put ice directly on the skin. Medications. Oral nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may be prescribed. In some cases, oral or injected steroid medications may be used in combination with immobilization to reduce pain and inflammation. Physical therapy. Physical therapy may be prescribed, including exercises and treatments to strengthen the muscles and decrease inflammation. The exercises may also help prevent recurrence of the symptoms. Orthotic devices. Custom orthotic devices that fit into the shoe provide support for the arch, and may play a role in preventing future symptoms. Even after successful treatment, the symptoms of accessory navicular syndrome sometimes reappear. When this happens, non-surgical approaches are usually repeated. Surgical Treatment In the original Kidner procedure, the entire posterior tibial tendon was released from the navicular and then rerouted through a drill hole placed through the navicular. The original Kidner procedure is now rarely used as a means of treating an isolated accessory navicular. Instead, a modification of the Kidner procedure has become more commonplace. The modified Kidner procedure consists of carefully removing the accessory and anchoring the posterior tibial tendon to the surface of the navicular where the accessory was removed. The repair may be done by passing a suture through the tendon and then through drill holes in the navicular, or by using a suture anchor. Overview
The human body is rarely the same from person to person. Some things stay the same, like the function of the internal organs. Even when structures are similar, however, little variations, like extra bone tissue, can make a significant difference in the body. Having small, extra bones is not as uncommon as you might think. Sometimes, though, these additional tissues can cause painful problems, as with accessory navicular syndrome.  Causes Accessory navicular syndrome as it is called can result from a number of causes, excess or overuse syndrome as seen in an athlete. Trauma to the foot as in an ankle sprain or direct trauma to the navicular bone. chronic irritation from shoes rubbing against the extra bone, over time, may cause pain. Excessive pronation which strains the attachment of tibialis posterior muscles into the navicular bone. Keep in mind, the larger the actual accessory bone, the greater the chance of it becoming an issue. Symptoms If you develop accessory navicular syndrome, you may experience a throbbing sensation or other types of pain in your midfoot or arch (especially while or right after you use the foot heavily, such as during exercise), and you may notice a bony prominence on the interior of your foot above the arch. This prominence may become inflamed, which means it will likely feel warm to the touch, look red and swollen, and will probably hurt. Diagnosis To diagnose accessory navicular syndrome, the foot and ankle surgeon will ask about symptoms and examine the foot, looking for skin irritation or swelling. The doctor may press on the bony prominence to assess the area for discomfort. Foot structure, muscle strength, joint motion, and the way the patient walks may also be evaluated. X-rays are usually ordered to confirm the diagnosis. If there is ongoing pain or inflammation, an MRI or other advanced imaging tests may be used to further evaluate the condition. Non Surgical Treatment Using PRP treatments, orthotics, proper running shoes and physical therapy should do the trick. No long recovery, no long down time. My runners and athletes are usually back to their sport pain free within a month. The key is eliminating the syndrome, not the bone (or cartilage).  Surgical Treatment If all nonsurgical measures fail and the fragment continues to be painful, surgery may be recommended. The most common procedure used to treat the symptomatic accessory navicular is the Kidner procedure. A small incision is made in the instep of the foot over the accessory navicular. The accessory navicular is then detached from the posterior tibial tendon and removed from the foot. The posterior tibial tendon is reattached to the remaining normal navicular. Following the procedure, the skin incision is closed with stitches, and a bulky bandage and splint are applied to the foot and ankle. You may need to use crutches for several days after surgery. Your stitches will be removed in 10 to 14 days (unless they are the absorbable type, which will not need to be taken out). You should be safe to be released to full activity in about six weeks. There are not one but two different kinds of leg length discrepancies, congenital and acquired. Congenital indicates that you are born with it. One leg is structurally shorter in comparison to the other. As a result of developmental periods of aging, the brain picks up on the walking pattern and identifies some difference. Your body usually adapts by dipping one shoulder to the "short" side. A difference of under a quarter inch isn't grossly uncommon, doesn't need Shoe Lifts to compensate and generally does not have a serious effect over a lifetime.
 Leg length inequality goes mainly undiscovered on a daily basis, however this condition is very easily fixed, and can eliminate a number of cases of chronic back pain. Therapy for leg length inequality typically involves Shoe Lifts. These are typically low-priced, generally costing below twenty dollars, in comparison to a custom orthotic of $200 or maybe more. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position. Lower back pain is the most prevalent condition affecting people today. Around 80 million men and women are afflicted by back pain at some stage in their life. It's a problem which costs businesses millions of dollars every year on account of time lost and productivity. New and superior treatment solutions are constantly sought after in the hope of reducing the economic impact this condition causes.  Men and women from all corners of the world suffer from foot ache as a result of leg length discrepancy. In these cases Shoe Lifts might be of beneficial. The lifts are capable of relieving any pain and discomfort in the feet. Shoe Lifts are recommended by numerous certified orthopaedic orthopedists. In order to support the human body in a well-balanced manner, the feet have a very important function to play. Irrespective of that, it is often the most overlooked zone of the body. Many people have flat-feet meaning there may be unequal force placed on the feet. This causes other body parts like knees, ankles and backs to be impacted too. Shoe Lifts guarantee that the right posture and balance are restored. There are not one but two different types of leg length discrepancies, congenital and acquired. Congenital indicates that you are born with it. One leg is anatomically shorter in comparison to the other. Through developmental periods of aging, the brain picks up on the gait pattern and identifies some variation. The body typically adapts by dipping one shoulder over to the "short" side. A difference of less than a quarter inch isn't very uncommon, doesn't need Shoe Lifts to compensate and ordinarily does not have a serious effect over a lifetime.
 Leg length inequality goes typically undiagnosed on a daily basis, yet this issue is easily corrected, and can reduce numerous instances of back pain. Treatment for leg length inequality usually consists of Shoe Lifts. These are typically cost-effective, in most cases being under twenty dollars, in comparison to a custom orthotic of $200 and up. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position. Chronic back pain is the most prevalent condition afflicting men and women today. Over 80 million people are affected by back pain at some point in their life. It's a problem that costs companies millions every year due to time lost and output. Fresh and more effective treatment solutions are continually sought after in the hope of reducing the economic influence this issue causes.  People from all corners of the world experience foot ache due to leg length discrepancy. In these types of situations Shoe Lifts are usually of very useful. The lifts are capable of eliminating any discomfort in the feet. Shoe Lifts are recommended by many qualified orthopaedic practitioners". To be able to support the body in a healthy and balanced manner, the feet have got a very important task to play. Irrespective of that, it is sometimes the most overlooked region in the body. Some people have flat-feet which means there may be unequal force placed on the feet. This causes other body parts including knees, ankles and backs to be impacted too. Shoe Lifts make sure that the right posture and balance are restored. |
|
